Disclaimer: the claims shared in this blog post are not my own, nor my opinion. They are science, research, evidence-based facts. I share them here since they are essential to understanding pain, and thus to treating it fully.
Learning about the existence of this model was a revelation and a validation to me, and I hope it will be for you too. I hope I can share it with you in a way that gives it sense, and is easy to comprehend. You will find references at the bottom.
WHAT IS PAIN?
“If you are someone living with pain and have only attempted to treat pain by targeting the body with pills and procedures, then you have NOT adequately treated your pain.” – Dr R. Zoffness
YOU HAVE A RIGHT TO UNDERSTAND PAIN
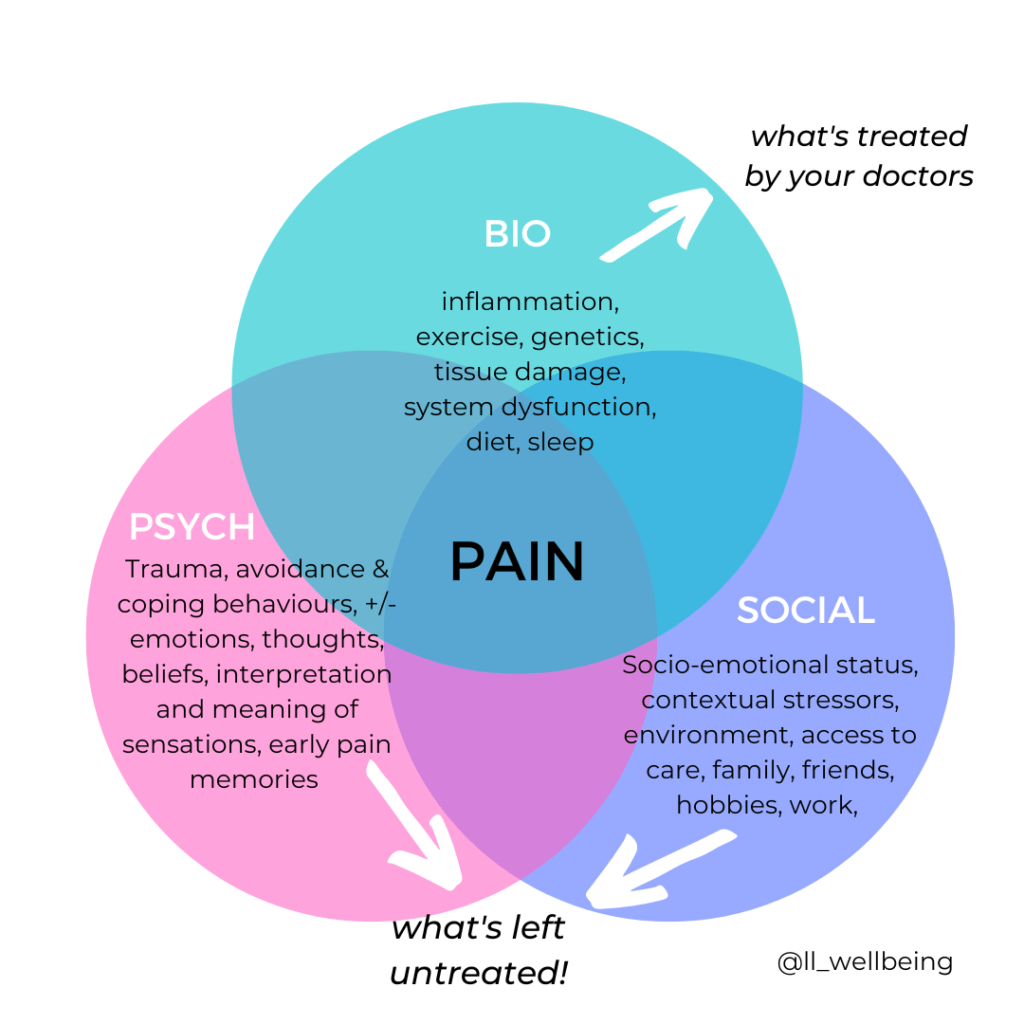
THE BIO-PSYCHOSOCIAL MODEL OF PAIN
There are 3 important components of pain. Treating one without the other, is just addressing only 1 part of the problem.
This is why in conditions like endometriosis, surgery alone will often lead to more pain.
I take this example in particular not only because it is a disease I know personally, but also because it is a condition that truly is visible in the body. There is tissue damage, visible by ultrasounds or MRI.
Yet, different women experience it very differently. For women that have suffered from pains for years before being diagnosed and finding validation, surgery alone is often not enough to get rid of all the pain.
PAIN IS BIOMEDICAL
That is the model that most of us experience when we seek help for chronic pain. The components of this model are:
- genetics,
- sleep,
- diet,
- exercise,
- tissue damage,
- system dysfunction
This is what our view of pain is reduced to. We are prescribed medications, or surgical procedures in order to fix this part, completely forgetting the other components of pain. We thus only treat ⅓ of the problem!
So what are the two other thirds?
PAIN IS PSYCHOLOGICAL
A good example of this is the fantom limb, where people who had a limb amputated can still feel the pain “in” it. This disturbing phenomenon shows that pain lives in the brain, and not anywhere else in the body! In fact, to his day, the best known treatment for fantom limb is to use a mirror between the amputee’s legs so that they can “see” two healthy legs, and “show” their brain that the leg is fine, thereby reprocessing the pain.
All pain is processed in the brain. Pain is constructed by the brain and the body.
There is not one single pain center in the brain; it is a diffuse neurological process, meaning many parts of the brain process this experience we call “pain” – Rachel Zoffness, PhD
There is a real biological connection between pain and emotion (Melzack & Wall, 1965):
Multiple parts of the brain are at play to process pain: the cerebral cortex, responsible for thoughts, the prefrontal cortex, responsible for attention and executive processing, and the limbic system, which is the emotion center. Together they produce this experience we call “pain”.
So pain is always informed by sensations and emotions; it is always emotional and physical at the same time, thus both the physical and the emotional must be dealt with in order to fully treat chronic pain.
This means we must target the brain in order to relieve the body!
PAIN IS SOCIAL/SOCIOLOGICAL
HOW DOES PAIN BECOME CHRONIC?
THE SENSITISATION PROCESS
Sensitisation happens through our Central Nervous System (otherwise called CNS= brain + spinal cord).
To explain this concept, think for example of a time where you got better at something by practicing it.
Here is mine:
Last month, my 10-year old daughter told me she would never be able to learn how to play the ukulele: her fingers hurt too much and she could not move them on the strings fast enough. Then she practiced for two weeks, and to everyone’s amazement, she was able to perform her first song soon after. Even her fingers did not hurt anymore!
This is because whatever we practice, we get better, stronger, faster at doing. Repetition is the key.
And so it is with our brain: the pathways in your brain are just like the muscles in your body: the more you use them, the bigger they get.
“Neurons that fire together wire together”, Head.
Overtime, the brain pathways that practice pain can grow bigger, more conducive and become more sensitive. They fire faster. They will overreact in a way similar to a fire alarm that is reacting to a burned casserole, or a car alarm that turns on when the wind blows. That is, the warning system is turned ON even when there is no danger.
RETAKE YOUR POWER WITHT HE PAIN DIAL
In our brain is some kind of a pain dial. When stress and anxiety are UP, our brain sends a message to the pain dial to increase pain volume. Thus the pain feels worse and lasts longer.
In that way negative moods and emotions matter and affect our perception of pain by making it worse. Think of how kicking your toe on a stone would feel different at a birthday party with friends, in opposition to after a long and stressful and frustrating day at work: would your experience of pain be the same?
When stress and anxiety are low, the brain sends a message to the pain dial to lower pain volume. The same is true with mood and emotions: pleasurable activities, happy mood, a distracted prefrontal cortex will also lower pain volume. Think of how a child receiving a vaccine is distracted by a movie or the promise of a candy.
Therefor there is a “recipe” for higher pain, and a recipe for lower pain days. What this really means is that YOU have the power to lower the pain volume. You just need to find the button!
Pain takes away power. But you can regain your power, your body and your life.
By learning how to use this pain dial, and understanding the science behind pain, you can regain a sense of agency over your life and body.
CONCLUSIONS
They are many things that you can do to change your pain. Your pain dial is your power.
YOU have the power to turn down the pain volume and make pain feel less bad.
And we can start today.
Because if it’s ok to go to a soccer coach to get better at soccer, surely it is ok to go to a pain coach to get better at LIVING WITH PAIN!
Living with pain is really hard and you deserve to understand it.
————————————————————————
Are you ready to take back your power?
Living with pain is hard. But you do not have to go at it alone! You deserve support.
The field of pain medicine is changing; come change it with me! Contact me today to find support and learn new ways to reduce pain volume, and feel energised to rebuild a life of joy, passion and fulfillment.